Introduction
Acinetobacter spp plays a significant role in the colonization and infection of patients admitted to hospitals.1 It typically colonizes skin, the respiratory, urinary, gastrointestinal tract, wounds and indwelling plastic devices of the hospitalized patients and can cause infections in burn, trauma, mechanically ventilated and immunocompromised patients. It shows a special predilection for the ICU.2
Multidrug resistant A. baumannii (MDR A. baumannii), defined as an A. baumannii strains resistant to at least three different antibiotic groups; penicillins and cephalosporins (including inhibitor combinations), fluoroquinolones, and aminoglycosides, has emerged and has been reported worldwide to significantly increase the morbidity, mortality, and cost of treatment. Acinetobacter spp. exhibit multidrug resistance through production of beta lactamases, alterations in outer membrane proteins (OMPs) and penicillin-binding proteins (PBPs), and increased activity of efflux pumps. Resistance to 𝛽-lactams appears to be primarily caused by production of 𝛽-lactamases which include extended-spectrum-𝛽-lactamases (ESBLs), metallo-𝛽-lactamases (MBLs), and oxacillinases.3
Metallo-beta-lactamases (MBL) are carbapenemases, belonging to Ambler class B that confers resistance to all beta lactam antibiotics except monobactams.4 They are not inhibited by clavulanic acid, tazobactam, or sulbactam; hence beta-lactam combinations with the currently available beta-lactamase inhibitors are not useful.5 Apart from their broad spectrum of activity, another factor causing concern is that many of the MBL genes may be located on plasmids with genes encoding other antibiotic resistance determinants, i.e., aminoglycoside resistance genes. These MBL-positive strains are usually resistant to beta-lactams, aminoglycosides, and fluoroquinolones.6 There are no clinically approved MBL inhibitors, making these enzymes a serious threat to human health.7
MBL prevalence among Acinetobacter spp ranged from 14 to 83% in various studies worldwide.8,9,10,11,12,13,14,15,16 The foremost implication of infection with carbapenem resistant A. baumannii is the need to use “last-line" antibiotics such as colistin, polymyxin B, or Tigecycline.17
With global increase in the occurrence and types of MBLs early detection is essential for implementing appropriate antibiotic therapy as well as infection control practices. Keeping this in view, the present study was undertaken to determine the prevalence of metallo-beta-lactamase producing strains of Acinetobacter spp in our hospital, and their antibiotic sensitivity pattern, so that appropriate infection control strategy and antibiotic policy can be formulated to prevent their spread.
Materials and Methods
57 non repetitive, clinically significant isolates of Acinetobacter spp. obtained during a one year period were subjected to antibiotic susceptibility testing by employing Kirby Bauer disc diffusion techniques according to CLSI guidelines. The isolates showing resistance to carbapenems (imipenem or meropenem) were subjected to screening test for MBL production: Screening tests for MBL:
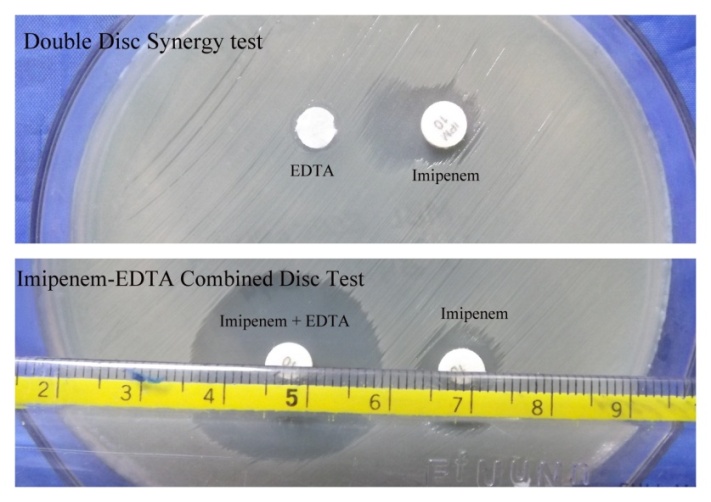
Imipenem and Imipenem-EDTA combined disc test (CDT)
The IMP-EDTA combined disc test was performed as described by Yong et al.18 Test organisms were inoculated as lawn culture on to plates with Mueller Hinton agar. Two 10 μg imipenem disks (Himedia) were placed on the plate, and appropriate amounts of 10 μL of 0.5M EDTA solution were added to one of them to obtain the desired concentration (750μg). The inhibition zones of the Imipenem and Imipenem-EDTA discs were compared after 16 to 18 hours of incubation in air at 35°C. If the increase in inhibition zone with the Imipenem and EDTA disc was ≥ 7 mm than the Imipenem disc alone, it was considered as MBL positive. (Figure 1)
Double disc synergy test (DDST)
The test organisms were inoculated as lawn culture on to plates with Mueller Hinton agar. An imipenem (10 μg) disc was placed 20 mm centre to centre from a blank disc containing 10 μL of 0.5 M EDTA (750 μg). Enhancement of the zone of inhibition in the area between imipenem and the EDTA disc in comparison with the zone of inhibition on the far side of the drug was interpreted as a positive result. (Figure 1)
Confirmatory test for MBL: E-test (Figure 2)
Isolates positive for MBL by either or both of the screening tests were confirmed by MBL E-test. The E Test MBL strip (Biomérieux) contains a double sided seven-dilution range of imipenem (4 to 256 μg /mL) and imipenem (1 to 64 μg /mL) in combination with a fixed concentration of EDTA. The E-test was done according to manufacturer’s instructions. The test was considered positive if it satisfied any of the following criteria
1. MIC ratio of IP (Imipenem)/IPI (Imipenem-EDTA) of >8 or >3 log2
2. Appearance of phantom zone
3. Deformation of the elliptical zone of inhibition.
Results and Discussion
Of the 57 isolates of Acinetobacter spp., 35% were from pus samples, 35% from respiratory specimen (sputum and suction tip), 14% from urine samples, 12.3% from blood and 1.8% from ear discharge and pleural fluid, each.
Majority of the isolates were obtained from the wards (49%) and ICUs (44%), the rest being from the OPDs (7%).
Of the 57 isolates, carbapenem resistance was recorded in 39 isolates. Screening tests for MBL showed 24 to be positive by CDT and 16 to be positive by DDST. All the 16 isolates which tested MBL positive by DDST were also positive by CDT. However CDT showed an additional 8 isolates to be MBL positive, as compared to DDST.
All 24 of the Acinetobacter spp isolates that tested MBL positive by the screening test showed positive result by E-test as well. Hence, the prevalence of confirmed MBL by E-test among Acinetobacter spp was found to be 42.2%.
50% of the pus samples (10 out of 20), suction tip samples (10 out of 20) and catheter urine samples (5 out of 10) tested positive for MBL. Sputum samples tested 40% (4 of 10) positive, urine 33.3% (2 of 6), and blood 28.6% (2 of 7).
Comparison of the sensitivity pattern of the MBL positive isolates with that of the MBL negative isolates (Table 1) showed statistically significant difference (P<0.05) for Cephalosporins, piperacillin, piperacillin tazobactam, carbapenems, aztreonam, fluoroquinolones and gentamicin. Colistin was found to be sensitive among all the MBL positive strains.
No statistically significant relation was found between the prevalence of MBL and age group, sex or history of antibiotic intake.
Table 1
Comparison of antibiotic sensitivity patterns of MBLS positive isolates with MBL negative isolates
Table 2
Comparison of MBL prevalence among acinetobacter spp with other studies
Discussion
Clinical isolates of Acinetobacter species initially retained at least partial susceptibility against the 3rd and 4th generations viz cephalosporins, fluoroquinolones, semisynthetic aminoglycosides, carbapenems and 100% susceptibility to imipenem but the clinical utility of this class of antimicrobial is increasingly being jeopardized by the emergence of both enzymatic and membrane-based mechanisms of resistance. The increase in the number of MBLs in A.baumannii is an ominous development in the global emergence of resistance to β-lactams.17
Carbapenem resistance among Acinetobacter spp was found to be 68.4% (39/57). Other published data indicate a widely varying range of carbapenem resistance among Acinetobacter spp, ranging from 23% to 99%.8,9,10,11,12,13,19
Of the 39 isolates showing carbapenem resistance, 24 were found to be by MBL production. For the remaining 15 isolates, resistance to carbapenems in the absence of class B metallo ß lactamase enzyme (MBL) production can be attributed to the production of other enzymes like Carbapenemase, Oxacillinase or to nonenzymatic mechanisms, including changes in outer membrane proteins (OMPs), multidrug efflux pumps and alterations in the affinity or expression of penicillin-binding proteins.20,21,22
The prevalence of MBL among Acinetobacter spp was found to be 42.2% in the present study which is comparable to the reports of Goel V et al10 and Amandeep Kaur et al.23 (Table 2)
The MBL isolates, in addition to resistance to cephalosporins and carbapenems, showed statistically significant resistance to fluoroquinolones and aminoglycosides. This could be explained by the concurrent carriage of resistance genes to aminoglycosides and fluoroquinolones on the same mobile genetic elements carrying the MBL gene.6
Colistin showed 100% susceptibility among the MBL positive isolates in this study, and hence can be considered to be a treatment option. However this drug has to be used judiciously as various reports of colistin resistant MBL Acinetobacter isolates have emerged.7,17,23 The emergence of colistin resistance can be attributed to selection caused by routine use of colistin as a first–line drug for severe nosocomial infections.24
Conclusion
In conclusion, this study has documented the prevalence of MBL production among Acinetobacter spp as 42.2%, in our hospital. The early detection of MBL-producing isolates is important for the reduction of mortality rates of infected patients and also to avoid the intra hospital dissemination of such strains. CDT using imipenem can be used as a convenient screening method for detection of MBL production in gram negative bacilli in routine Microbiology laboratory where molecular methods are not feasible. At present, Colistin appears to be a suitable treatment option for MBL positive Acinetobacter spp, however, it should be used judiciously to prevent emergence of resistance. Continuous monitoring of MBL prevalence and formulation of appropriate antibiotic policy is the need of the hour for surveillance and control of MBL in the hospital.