Introduction
Dermatophytosis is the most important group of superficial fungal infections caused by dermatophytes, which is a group of fungi that are capable of growing by invading the keratin of skin, hair, and nail for obtaining nutrients. There are several reports on intracontinental variability of the global incidence because of the change in climatic condition across the world.1
According to World Health Organization (WHO), the prevalence rate of superficial mycotic infection worldwide has been found to be 20-25%.2 It is more prevalent in tropical and subtropical countries like India where the heat and humidity is high for most part of the year.3
Environmental factors include high temperature and relative humidity, which provide conditions favourable to fungal dispersion and development. Sociodemographic factors, such as poor socioeconomic status, promiscuity, prolonged contact with animals, and poor hygiene conditions, are also conducive to the incidence and propagation of mycotic infections.4
Dermatophytes include several genera like Trichophyton, Microsporum, and Epidermophyton. Some common organisms include Trichophyton Sudanese, Trichophyton tonsurans, Trichophyton verrucous, Trichophyton rubrum, and Microsporum canis.5
Clinical manifestations vary depending on the causal agent and on the host immune response; they may last months or years, and may be asymptomatic or manifest only as pruritus.6
The diagnostic tests include potassium hydroxide (KOH) wet mount examination, wood’s lamp examination, skin biopsy and fungal culture.7
Another method for confirmation is a fungal culture. Fungal cultures are possible but take time for definitive identification. Cultures may begin to see growth in about five days but may take up to four weeks in certain species. Therefore, at least four weeks are needed to deem a sample as "no growth." The most common isolation medium used for fungal cultures is a Sabourad dextrose agar (1% glucose, 4% mycological peptone agar, water). Identification is by examining the morphology, pigmentation, and surface topography of the culture.8
The present study was undertaken to assess the clinical profile of dermatophytic infections and to identify the causative fungal species in various clinical presentations among the patients attending the dermatology department of Katuri Medical College and Hospital, Guntur, Andhra Pradesh.
Materials and Methods
Study participants
Suspected cases of dermatophytosis attending the outpatient department of Dermatology, KMC&H, Chinakondrupadu, Guntur.
Sample size
The sample size for the present study was estimated based on prevalence of Dermatophytic infections in India i.e. 27.6% as the study conducted by Lakshmanan et al.,9
Sample size estimation formula:
n= sample size, z = 3.84 at 95% Confidence Interval, d = Absolute Precision, = 7%
p = prevalence, substituting the values in above formula, the minimum sample size for the study was estimated to be 157 which was approximated to 163.
163 clinically suspected cases of dermatophytosis attending the outpatient department of a tertiary care hospital during January 2018 to May 2019 were randomly selected for the study. Ethical clearance was obtained from the Institutional Ethical Committee prior to the start of the study.
A detailed history and clinical examination was done. Details of skin lesions were noted. Complete blood picture, blood glucose levels, renal function tests were done for all patients. Patients were referred to the ICTC for HIV testing whenever suspected.
Exclusion criteria
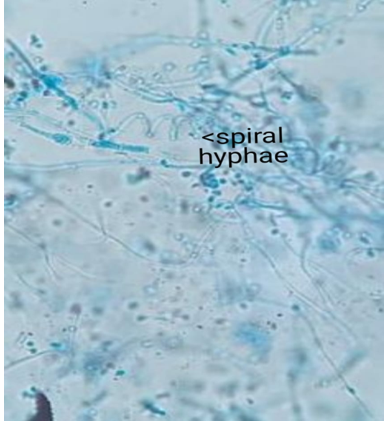
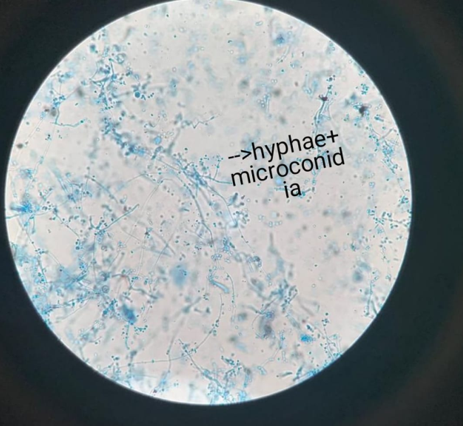
Depending on the presenting condition skin scales, crusts, nail clippings, or easily pluckable hair were collected in clean white paper packets. Specimen collected was subjected to potassium-hydroxide (KOH) wet preparation (10% KOH for skin and hair; 40% KOH for nail) for the presence of fungal elements. After direct microscopic examination, irrespective of demonstration of fungal elements, the specimen was inoculated into a test tube containing Sabouraud's dextrose agar with 0.05% chloramphenicol and 0.5% cycloheximide. This was incubated at 28°C for up to 4 weeks. If no growth was found after 4 weeks, it was taken as negative for growth of fungi. Fungal isolates were identified based on colony morphology, pigmentation, growth rate, microscopy (Lactophenol Cotton Blue mount), and slide culture. Special tests were done when necessary, namely, hair perforation test and urease test for species identification.
Results
Out of 163 cases, 73 (44.79%) were males and 90 (55.21%) were females. Male-to-female ratio was 0.81:1. Majority of the patients belonged to the age group of 31 – 40 years (23.93%) followed by 21 – 30 years age group (20.86%) (Table 1).
Majority of male belong to the age group of 21 – 30 years (23.29%) where asmajority in female belonged to 31 – 40 years age group (Table 1).
Table 1
Age and gender distribution
According to Modified B G prasad scale of socioeconomic status classification (May 2019 update), majority belonged to lower class (34.36%) followed by upper lower class (28.83%).
Table 2
Clinical type and gender distribution
Out of the 163 patients studied, Tinea corporis was the most common clinical type observed among95 cases (58.28%). Among males, incidence of T. corporis was observed to be high compared to other clinical types with 63.01% among males and 58.28% among female(Table 2).
Distribution of other clinical types among male, T cruris (2.74%), T faciei (1.37%), T mannum (1.37%), T pedis (1.37%), T capitis (1.37%), Mixed infections (28.77%) (Table 2).
Distribution of other clinical types among Female, T cruris (3.33%), T faciei (1.11%), T mannum (1.11%), T pedis (2.22%), T capitis (1.11%), Mixed infections (36.67%) (Table 2).
Table 3
Mixed dermatophytoses
In the present study, out of 163 cases studied Mixed dermatophytosis was observed in 54(33.13%) cases. Out of which majority were T corporis + T cruris (66.67%) clinical types (Table 3).
Table 4
Species wise distribution of dermatophytosis and their clinical presentation
In the present study, 33.12% of the cases showed culture positive isolates. Out of the 95 cases with T corporis, 16.84% were culture positive isolates. 66.6% of the mixed infections showed culture positive isolates (Table 4).
Table 5
Culture positive isolates and species wise distribution
|
|
Contaminants |
No growth |
T.r |
T. m |
T.t |
M.g |
M.a |
|
Skin |
2 |
22 |
7 |
39 |
2 |
3 |
1 |
|
Hair |
2 |
23 |
Nil |
Nil |
Nil |
Nil |
Nil |
|
Nail |
6 |
54 |
Nil |
2 |
Nil |
Nil |
Nil |
|
Total |
10 |
99 |
7 |
41 |
2 |
3 |
1 |
On the basis of culture characteristics, out of 54 culture positive samples T. mentagrophytes was the commonest (78.8%), followed by Tricchophyton rubrum (12.96%), Microsporumgypseum (11.11%), Trichophyton tonsurans (3.70%), Microsporumaudouinii (1.85%) (Table 5).
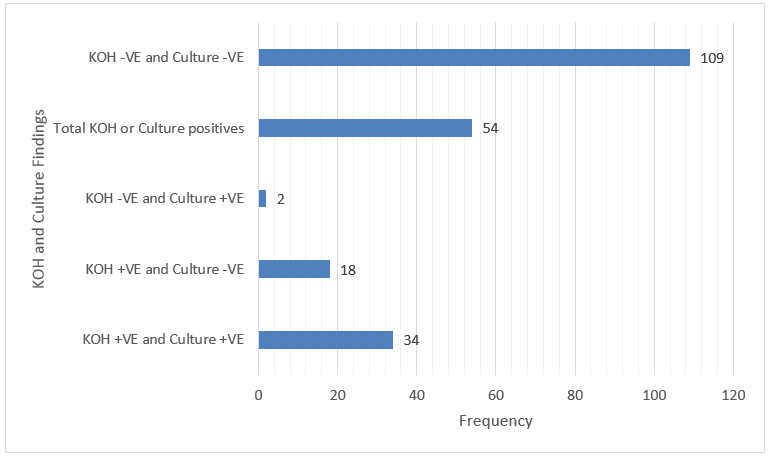
Out of 163 samples, total KOH and/or culture positive samples are 54. The following are the KOH and culture findings (Table 6).
Discussion
In the present study, majority i.e. 90 (55.21%) were females and 73 (44.79%) were males with a Male-to-female ratio of 0.81:1. Similar findings were observed in study conducted by Sudip Das et al.,10 where out of 103 cases of clinical dermatophyte infection were studied, 66 (64%) female and 37 (36%) male patients. The higher incidence in female is due to the poor hygienic conditions and increased wet work in case of housewives.
In contrary study conducted by Noronha et al.,11 and Janardhan et al.,12 showed incidence of dermatophytoses was more in male than female.
Majority of the participants are in the young age group i.e. within 20 – 40 years age groupin the present study. The Higher incidence in young age group is due to the greater physical activity with increased seating and increased opportunity for exposure. This finding was Similar compared to study conducted by Noronha et al.,11 Janardhan et al.,12 Sudip Das et al.,10
Based on Socio-Economic status majority belonged to lower class (34.36%) followed by upper lower class (28.83%) in the present study. Due to poor sanitation and hygienic conditions the incidence is higher. Similar findings were observed in study by Noronha et al.,11 where the study reported out of 150 participants, 92 (61.3%) were poor, 26 (17.3%) belonged to the lower middle class, 26 (17.3%) were below poverty line, and 6 (4%) belonged to the upper middle class.
Tinea corporis was the most common clinical typereported in the study by Janardhan et al., 12 Noronha et al.,11 Sudip Das et al.,10 which is similar to the present study findings.
Tinea corporis was most common due to the affinity of certain species for particular anatomical site.
Gupta et al.,13 reported that T.corporis+T.cruris were the most common clinical type which is in agreement with the present study findings.
In the present study, the cases who were on steroids observed to have masked Tinea infection as observed in culture.
T. mentagrophytes was the commonest (78.8%) dermatophyte observed in the culture isolates which is similar to the study conducted by Noronha et al.,11 In contrary, T rubrum was the common isolate in the study conducted by Janardhan et al.,12 and Sudip Das et al.,10 These differences may be due to the regional variation in the prevalence of various dermatophye species.
In the present study, Out of 163 samples, total KOH and/or culture positive samples are 54. The variations seen in the HOH and culture findings in the present study have been reported in the study by Sumana V et al.,14 This could be due to the non-viability of fungal elements in few cases.
Conclusions
The present study shows that dermatophyte infection was found to be higher in younger age group especially in females. Tinea corporis was the most common clinical type followed by T corporis + T cruris. The infection was found to be higher among lower socio-economic class.
Also, the present study gives an insight about the aetiological agents of dermatophytosis in the part of KM & CH, Chinakondrupadu. Trichophyton mentagrophytes was implicated as the predominant species followed T rubrum. Most Indian studies have reported T rubrum as the predominant isolate from dermatophytosis. So, the present study reveals the changing trends in the prevalence of various dermatophyte species in this area.
Finally, this data could help in the diagnosis of the disease and thus the spread of the disease can be controlled with specific control measures.