- Visibility 173 Views
- Downloads 15 Downloads
- DOI 10.18231/j.ijmr.2021.066
-
CrossMark
- Citation
Desmoplastic ameloblastoma in maxilla mimicking fibro-osseous leison: A case report
- Author Details:
-
Sonia Bai JK *
-
Midhun N
-
Divyasree M
-
S Aravind Kumar
-
Poornima P
Introduction
Ameloblastoma is the second most common benign epithelial odontogenic tumor.[1] Desomoplastic ameloblastoma (DA), a rare histologic variant of solid multicystic ameloblastoma was first reported in 1981 and detailed report was given by Eversole and his coworkers in 1984.[2] In 2017, world health organization has included Desmoplastic variant in follicular pattern and not as a separate clinicopathological entity.[3] The origin of the tumor is either from the epithelial rests of malassez or from the oxytalan fibres of the periodontal membrane.[4] Most of the desmoplastic variant of ameloblastoma usually appears in the maxilla showing mixed radiolucency and radiopacity with diffused surrounding features and resembling a benign fibro-osseous lesion. A differential diagnosis between the osteoplastic variant of desmoplastic ameloblastoma and fibro-osseous lesions such as fibrous dysplasia or ossifying fibroma can be very difficult.
Case Report
A 22-year old female patient has reported to the dental OPD complaining of pain and swelling in the maxillary anterior region. The swelling is gradually progressive and is on sudden onset with duration of one month. Extra oral examination did not reveal any asymmetry and the findings were non- contributory ([Figure 1]). Intra oral examination revealed swelling in the maxillary anterior region which is oval in shape with normal colour, firm in consistency and tender in nature. Mucosa over the swelling was normal, with no surface changes, no sinus openings or discharge. The mass was approximately 3.0 x 4.0 cms in diameter extending anterio-posteriorly obliterating the labial vestibule to marginal gingiva of 22and 23 and mesio-distally extending from 21 to 23. ([Figure 2])



Radiographic examination of an intraoral peri apical radiograph showed mixed radio-opacity and radiolucency with respect to 22 and 23. The mass has displaced the roots of lateral incisor and canine (22 23). The maxillary occlusal radiograph revealed a diffuse, ill-defined predominantly radio lucent lesion interspersed with fine radio opaque areas extending from distal aspect of left lateral incisor to the mesial aspect of left canine with displacement of roots. Based on the clinical and radiographic location, provisional diagnosis of desmoplastic ameloblastoma was made with ossifying fibroma, calcifying epithelial odontogenic tumor, Adenomatoid odontogenic tumor in the differential diagnosis.
An excisional biopsy was performed by marginal resection. Gross specimen with the size of 2.0 cm × 1.3 cm × 0.7 cm was received in formalin for histopathology. The specimen was soft to hard in consistency, irregular in shape, brown in colour. Specimen was cut into two parts named as A1 and A2.
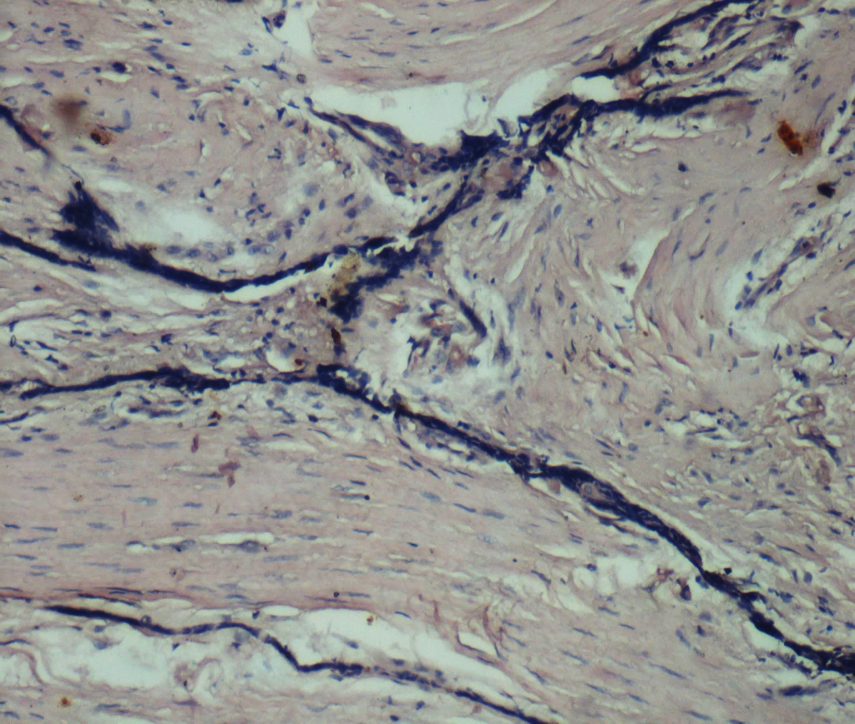
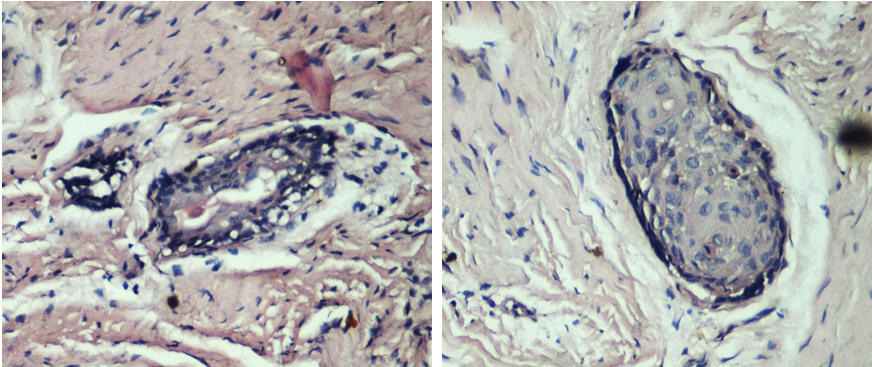
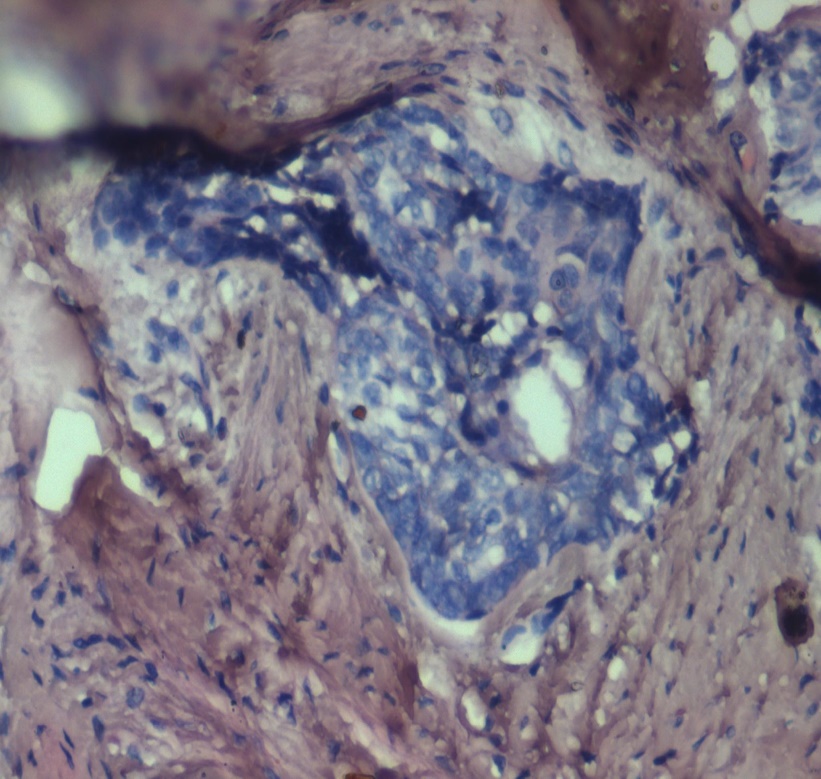
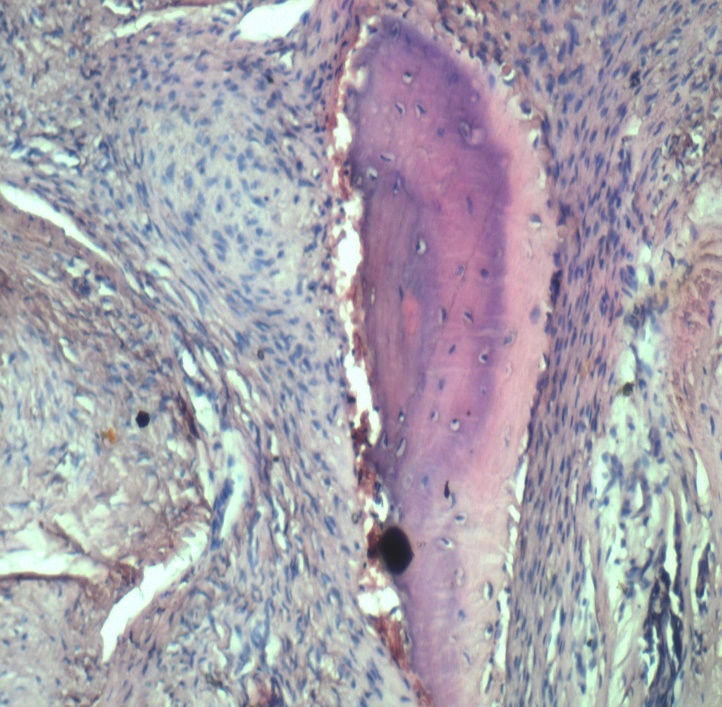
Histopathological examination of H and E - stained sections showed dense fibrous connective tissue surrounding the tumor islands (Fig. 5a and b). These tumor islands were connected in the form of interlacing strands. Some of them were in the form of follicles of varying size; some follicles showed squamous metaplasia in few areas (Fig. 6). Blood vessels and extravasated RBC’s were also seen. The biopsy led to the diagnosis as DA. Further the patient underwent surgical excision. The case was followed up for one year which revealed that there was no residual tumor or recurrence.
Discussion
Desmoplastic ameloblastoma (DA) is an benign epithelial odontogenic tumor which was first described by Eversole in 1984. In 2005, desmoplastic ameloblastoma has been considered as a distinct entity from conventional ameloblastoma. DA differs strikingly in its clinical, radiological and histopathological presentation when compared to other variants of ameloblastoma. [5] In 2017, WHO has divided Ameloblastoma into four categories; conventional, extraosseous / peripheral, unicystic, and metastasizing ameloblastoma. [6] Conventional ameloblastoma usually shows slow, painless expansion with the posterior area of mandible as the most common location whereas Only the desmoplastic type has different clinical features, including mixed radiolucent and radioopacity appearance, and predilection for the anterior jaws, especially maxilla.[7] This mixed radiolucent and radioopacity appearance with diffused borders provides a radiographic differentiation between desmoplastic ameloblastoma and fibro-osseous lesions.[8] The three radiological presentations of DA are are Type I (Osteo-fibrosis type): radiolucent as well as radiopaque appearance; Type II (Radiolucent type): completely radiolucent appearance; and Type III (Compound type): radiolucent as well as radiopaque combined with large radiolucent change.[8] According to this, our case had radiographic features similar to type III in which the unilocular radiolucent lesion developed subsequently adjacent to the mixed radiopaque-radiolucent lesion. This unusual radiographic appearance of DA could be because of the presence of the residual bone or due to new bone formation. Histologically, irregular odontogenic islands, with a stretched-out 'kite-tail' appearance are seen in a dense desmoplastic stroma. The peripheral layer of the epithelial islands was made up of flattened cells and the inner core was made up of spindle-shaped and, in some instances, squamous-shaped cells.[9] An Excisional biopsy was performed to establish the definitive diagnosis. Before biopsy, routine blood investigations were done which came out to be within normal limits. Histopathologically H&E stained sections showed odontogenic epithelial islands and cords scattered in a pronounced desmoplastic stroma. Connective tissue stroma consisted of dense collagen fibers and seemed to compress the odontogenic epithelial islands which shows kite-tail appearance. Areas of new bone production with osteoblastic rimming were also seen within the lesional area. Reports have stated that the tumors in the anterior jaws may mature sooner than those in the posterior region. Also, most of the cases of DA are known to have ill-defined margins and as a result, the chances of recurrence are more common than conventional ameloblastomas. Long term timely follow up of the case should be done in order to prevent post surgical recurrence.[10]
Conclusion
The desmoplastic ameloblastoma, a variant of conventional ameloblastoma is characterized by specific clinical, radiographic, and histological features. Long term follow up is required for proper understanding of cases. The clinician has to be alert regarding the unusual presentation of this neoplasm and should include desmoplastic ameloblastoma as differential diagnosis in any lesion ranging from simple abscess to any fibro-osseous lesions. The definite diagnosis requires histopathological examination. Also with the potential for recurrence, such cases should always be treated by complete resection.
Source of Funding
None.
Conflict of Interest
The authors declare no conflict of interest.
References
- PM Desai, M Khorate, N Figueiredo. Desmoplastic ameloblastoma of the mandible: A rare case report. Med Radiol 2020. [Google Scholar]
- MC Shashikanth, MC Neetha, M Ali, P Shambulingappa. Desmoplastic ameloblastoma in the maxilla: a case report and review of literature. Indian J Dent Res 2007. [Google Scholar]
- JM Wright, MS Tekkesin. Odontogenic tumors: where are we in 2017 ?. J Istanb Univ Fac Dent 2017. [Google Scholar]
- S Kulkarni, I Mohtesham, D Karteek. Desmoplastic Ameloblastoma: A case report with a brief review. J Dent Oral Res 2018. [Google Scholar]
- D Khurana, A Thakur, S Kadam, JV Tupkari. Desmoplastic Ameloblastoma-An unusual presentation. J Oral Med Oral Surg Oral Pathol Oral Radiol 2017. [Google Scholar]
- JM Wright, M Vered. Update from the 4th Edition of the World Health Organization Classification of Head and Neck Tumours: Odontogenic and Maxillofacial Bone Tumors. Head Neck Pathol 2017. [Google Scholar]
- HP Philipsen, PA Reichart, T Takata. Desmoplastic ameloblastoma (including “hybrid” lesion of ameloblastoma). Biological profile based on 100 cases from the literature and own files. Oral Oncol 2001. [Google Scholar]
- AJ Lewis, S Dorai, K Boaz, N Srikant, M Baliga, D Poojary. Desmoplastic ameloblastoma: A report of three cases from a single institute with review of literature. Eur J Mol Clin Med 2021. [Google Scholar]
- A Imran, SA Kumar, Sriram, SM Kumar. Desmoplastic ameloblastoma. CHRISMED J Health Res 2016. [Google Scholar]
- R Shetty, SV Sreelatha, P Hegde, P Shetty. Desmoplastic Ameloblastoma- A case report. Int J Adv Res 2017. [Google Scholar]
How to Cite This Article
Vancouver
JK SB, N M, M D, Kumar SA, P P. Desmoplastic ameloblastoma in maxilla mimicking fibro-osseous leison: A case report [Internet]. Indian J Microbiol Res. 2021 [cited 2025 Sep 12];8(4):333-336. Available from: https://doi.org/10.18231/j.ijmr.2021.066
APA
JK, S. B., N, M., M, D., Kumar, S. A., P, P. (2021). Desmoplastic ameloblastoma in maxilla mimicking fibro-osseous leison: A case report. Indian J Microbiol Res, 8(4), 333-336. https://doi.org/10.18231/j.ijmr.2021.066
MLA
JK, Sonia Bai, N, Midhun, M, Divyasree, Kumar, S Aravind, P, Poornima. "Desmoplastic ameloblastoma in maxilla mimicking fibro-osseous leison: A case report." Indian J Microbiol Res, vol. 8, no. 4, 2021, pp. 333-336. https://doi.org/10.18231/j.ijmr.2021.066
Chicago
JK, S. B., N, M., M, D., Kumar, S. A., P, P.. "Desmoplastic ameloblastoma in maxilla mimicking fibro-osseous leison: A case report." Indian J Microbiol Res 8, no. 4 (2021): 333-336. https://doi.org/10.18231/j.ijmr.2021.066
